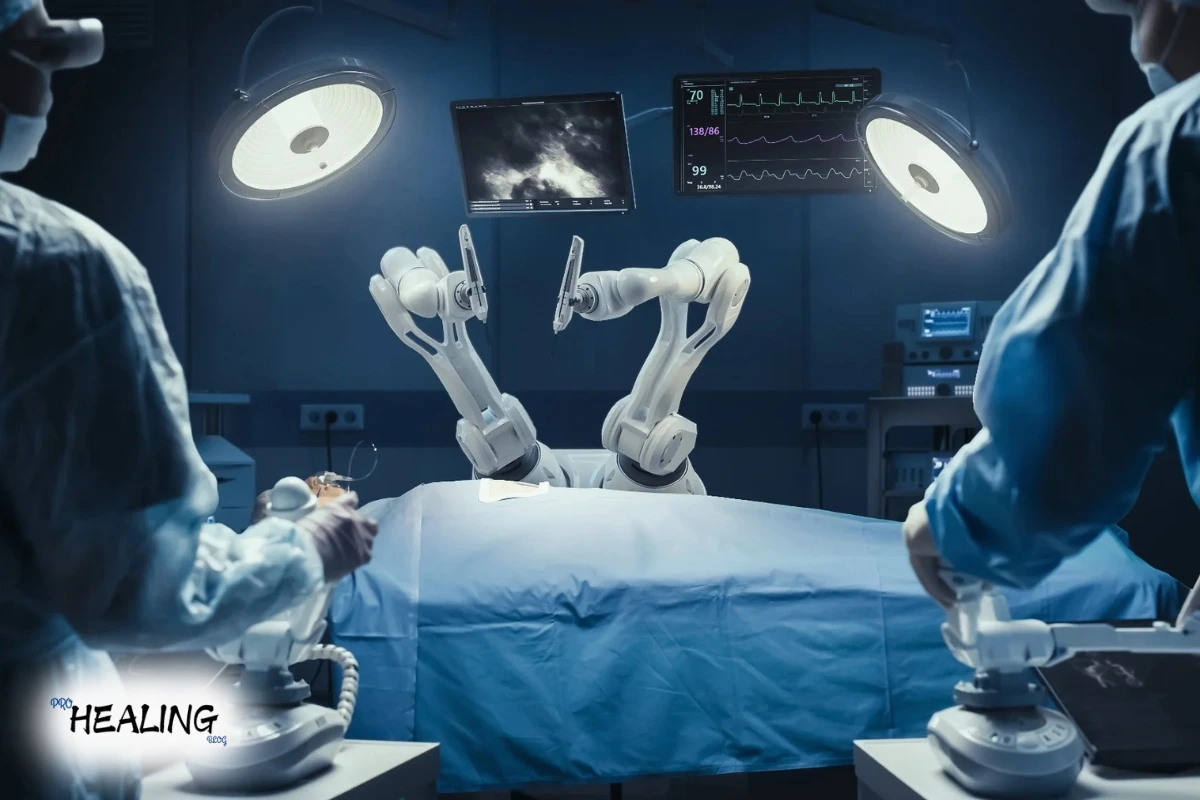
Autonomy in surgical robotics is an emerging area of research aimed at merging robotic systems with different degrees of autonomy in conducting surgical procedures. This shift in paradigm is significantly influenced by the increasing integration of artificial intelligence (AI) and machine learning (ML) with surgical technology.
While the majority of autonomous robotic systems are still in experimental stages, a considerable proportion have progressed into actual clinical applications. For instance, venipuncture, hair transplantation, anastomosis of the intestine, total knee arthroplasty, cochlear implantation, radiosurgery, and securing knots are representative of the autonomy capabilities of autonomous robotic surgery.
See Also: Why Is CPR Considered a Life Saving Technique?
Core Principles Behind Autonomy in Surgical Robotics
Two key elements for effective patient care are experience and knowledge. Generally, doctors develop both through practice and ongoing education. Nevertheless, as a result of time constraints, the human brain has a limitation in terms of processing vast amounts of medical information.
Thankfully, with the digital age, large sets of patient data can be accumulated and processed at unprecedented velocity. The fundamental objective of AI for surgical robotics is to leverage such sets of data so that systems can acquire “experience” many times quicker than any human being.
Consequently, using advanced algorithms, computer software is able to simulate—and surpass—human learning velocity. Autonomy in surgical robotics, therefore, allows machines to perform reasoning-based, problem-solving, and decision-making tasks using acquired information.
Role of Machine Learning in Surgical Robotics
Machine learning (ML), one of the constitutive elements of AI, is a major factor in surgical robotics autonomy. ML models learn over time by detecting patterns within past data to perform smarter and better tasks. Supervised learning, unsupervised learning, and reinforcement learning are among the algorithms that are being used more in robotic surgery for tasks that include diagnosis and surgical planning.
Furthermore, DL—a type of ML based on human neural networks—allows for surgical robots to process information by using several “hidden layers.” This enables them to derive detailed patterns, ultimately leading to best-case surgical results.
AI and ML in the Surgical Robotics Landscape
Now, AI enables autonomous motion in surgical robots. With increasing interest from the surgical community, particularly in fields such as general surgery, endoscopy, and interventional radiology, autonomy in surgical robotics is becoming increasingly mainstream.
Interestingly, ML is being applied in two main ways within the surgical domain: robotic task performance and decision support. It allows systems to forecast outcomes, aid in surgical planning, and detect possible postoperative complications—ultimately improving accuracy and patient safety.
Developmental Milestones in Autonomy in Surgical Robotics
The evolution of autonomy in surgical robotics consists of numerous worthy milestones. Devices have progressively evolved from completely manual robotic devices to systems that are able to make some decisions and even act alone under specific situations.
See Also: 8 Best Sleeping Accessories for 2025: Sleep Like Royalty
Following is a condensed list of robotic surgery milestones illustrating stages of autonomy (according to Yang et al.):
| Year | Milestone | Level of Autonomy |
|---|---|---|
| 1985 | PUMA 200 performs brain biopsies | Level 0 |
| 1989 | PROBOT for prostate surgery | Level 1 |
| 1992 | ROBODOC assists in hip replacement | Level 0 |
| 2000 | da Vinci System FDA-approved | Level 0 |
| 2001 | CyberKnife approved for radiosurgery | Level 2–3 |
| 2005 | ARTAS hair restoration system | Level 3 |
| 2016 | STAR performs standalone intestinal anastomosis | Level 3 |
Levels of Autonomy in Surgical Robotics
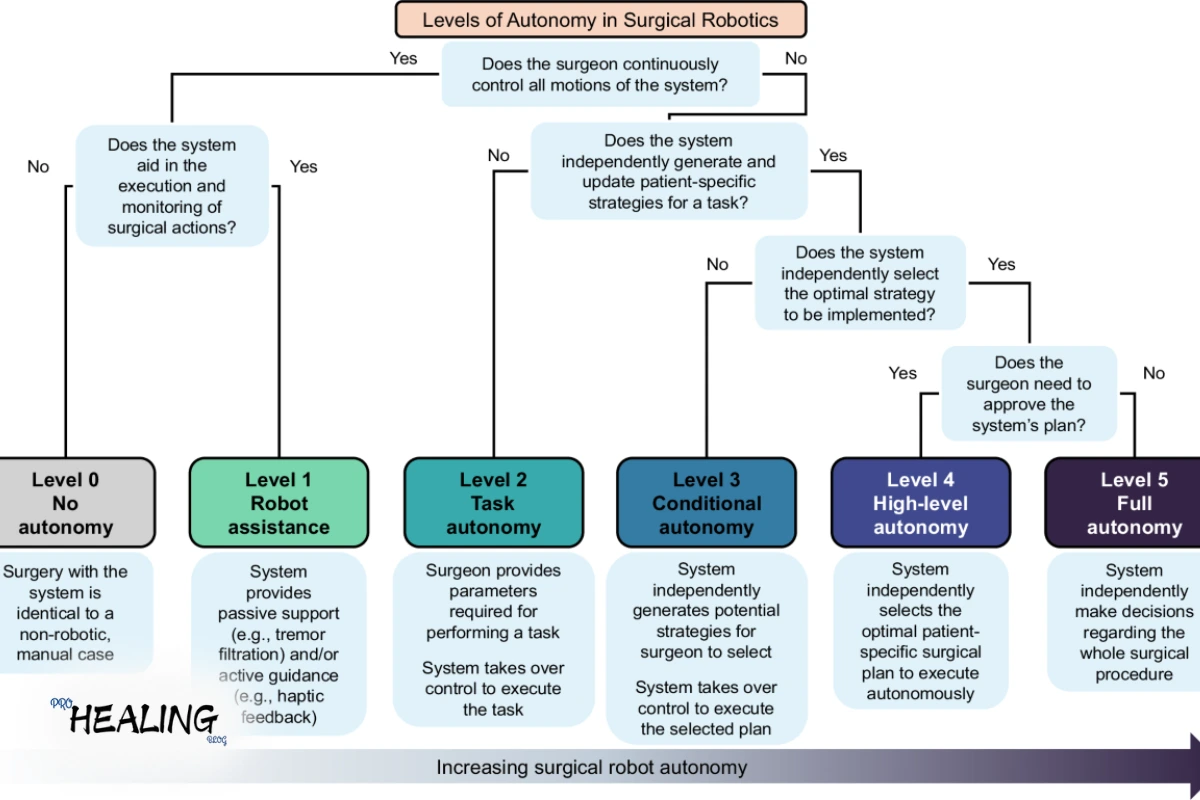
Yang et al. suggest that robotic surgical autonomy is divisible into six tiers:
-
Level 0: Full surgeon control; no automation
-
Level 1: Restricted assistive tasks (e.g., improved views or guidance)
-
Level 2: Robot performs set tasks at the direction of the surgeon within pre–programmed guidelines
-
Level 3: Robots plan and revise tasks in progress based on perception
-
Level 4: Systems autonomously execute entire surgical plans under human oversight
-
Level 5: Fully autonomous surgery with zero human input (currently unattained)
Current Applications of Autonomy in Surgical Robotics
The below-mentioned examples refer to the sophisticated application of autonomy in surgical robotics at Level 3:
-
STAR (Smart Tissue Autonomous Robot): Is superior in intestinal anastomosis.
-
TSolution One: Helps in bone preparation during joint replacements.
-
Veebot: Automates blood sample harvesting.
-
ARTAS System: Conducts graft harvesting in hair transplant surgeries.
-
CyberKnife: Performs radiosurgery with less human intervention.
Limitations of Autonomy in Surgical Robotics
Notwithstanding its promise, autonomy in surgical robotics is challenged by several issues:
-
Surgical Complexity: Autonomy is challenged by unexpected anatomy or emergencies.
-
Sensor Limitations: Low-quality data can compromise real-time decisions.
-
Ethical Concerns: Concerns regarding liability, accountability, and informed consent continue to develop.
-
High Costs: Robotic systems are still costly to develop and deploy.
-
Training Requirements: Systems need to be trained using large datasets for safety and reliability.
Thus, though robotic autonomy holds promise, clinical integration remains to need substantial safeguards and refinement.
See Also:Can You Freeze Avocados? The Ultimate Guide to Preserving Freshness
Legal and Ethical Dimensions of Surgical Robotic Autonomy
As surgical robotics becomes more autonomous, so too should the laws that regulate it. Ethical issues with liability, accountability, and culpability remain intricate.
-
Accountability: The black box nature of AI decision-making requires interventions such as explainable AI and black-box logging.
-
Civil Liability: Robots are not yet legally responsible for causing harm to patients.
-
Culpability: Robots are not conscious beings, so it is not possible to hold them legally culpable in the event of an error.
Finally, existing regulations are not fully prepared to cope with autonomous medical mistakes—implicating deeply into future malpractice suits.
Global Regulatory Landscape
Currently, large health agencies like the FDA (USA), MHRA (UK), and BfArM (Germany) have not yet developed frameworks specific to surgical robotics autonomy. Directives of reports like the EURON Robotics Roadmap imply that autonomous choices in surgery should always be backed by human observation in order to uphold ethical and clinical safety norms.
If Something Goes Wrong, Who Is Responsible?
Today, such devices as Intuitive Surgical‘s da Vinci robot leave final control in the hands of the surgeon, keeping the law as clear as possible. Surgeons in most jurisdictions are still responsible—despite a malfunctioning robot. Because the technology remains contingent on human initiation and oversight.
Will Robots Replace Surgeons?
Most professionals concur that surgical robotics autonomy is not a matter of replacing surgeons but assisting them. These systems are meant to offer greater precision, less fatigue, and better results—not to render the human expert obsolete.
Rather, the future is in collaborative autonomy, where human ingenuity and robotic accuracy combine to produce safer, more efficient surgery.
Conclusion
With advances in autonomy for surgical robotics, it promises to change the future of medicine. Even as technical, ethical, and regulatory issues continue, combining AI and ML with robotic surgery is changing the way surgeries are planned and carried out. From aiding in simple tasks to carrying out complicated operations, surgical robots that can perform autonomously are promising a future of smarter, safer, and more efficient healthcare.
See Also: Can You Freeze Avocados? The Ultimate Guide to Preserving Freshness